Around 5-10 million women seek gynecological advice for vaginal candidiasis across the globe. Vaginal candidiasis is an infection affecting women’s vagina. It is caused by the Candida group of fungi. Mostly, Candida albicans, a fungus normally present in the vagina that is often harmless, causes this fungal infection. However, when a woman’s immune system weakens, this fungus multiplies and produces symptoms. This is also known as a vaginal yeast infection or vaginal thrush.
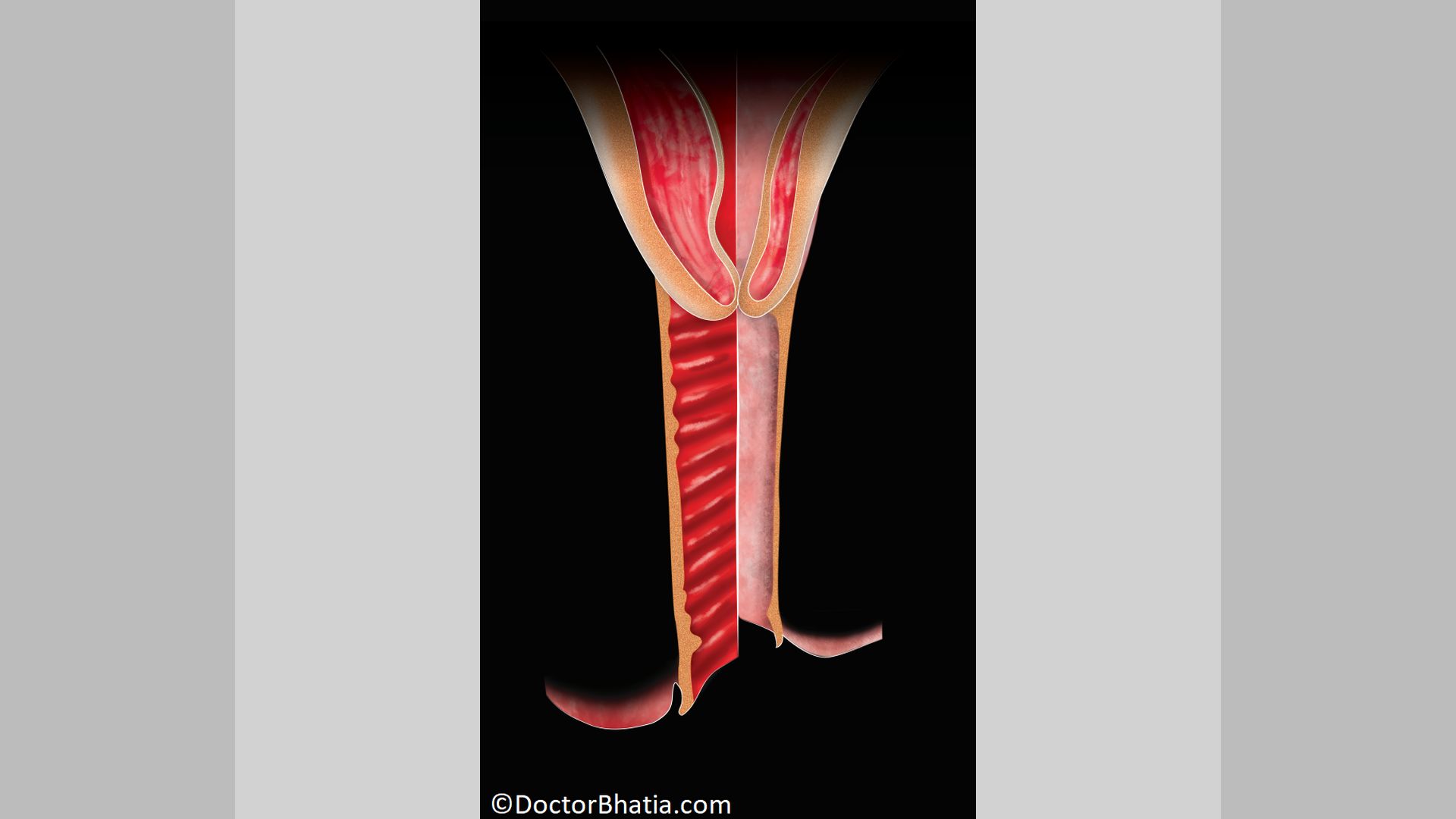
Vaginal candidiasis causes inflammation of the vulva and vagina. Cracks appear in the vagina due to this fungal infection. The symptoms of vaginal candidiasis include itching and vaginal discharge. This vaginal discharge can be thick or thin and mostly white-looking, like cottage cheese. Vaginal candidiasis is accompanied by pain, burning sensation while passing urine or Homeopathy not only stops the fungus from multiplying in the vagina but also prevents the recurrence of vaginal candidiasis.
Homeopathic medicines control the symptoms of vaginal candidiasis. They help treat vaginal candidiasis from its root by raising the body’s immunity. As the fungus growth reduces, the symptoms also wane off.
Role of homeopathy in vaginal candidiasis
A disruption in vaginal microbes causes vaginal candidiasis. Homeopathic medicines cure vaginal candidiasis by treating this root cause. However, the effectiveness of homeopathic medicine depends on the specific remedies chosen and the severity of the vaginal candidiasis. So consulting a qualified homeopath is essential to get the suitable remedies for your vaginal candidiasis.
Top five homeopathic medicines for vaginal candidiasis
Sepia officinalis (Sep.)
Common name: Inky juice of cuttlefish
Sepia is used for vaginal candidiasis with milky white discharge. These women often complain of excessive itching, excoriation in the vulva and vagina. The itching is so intense that even after scratching, it does not get relieved.
Sepia is indicated for vaginal candidiasis in menopausal women. The women who need Sepia have swelling and soreness of the labia minora, vulva, and vagina during vaginal candidiasis. There is marked heat felt in the genitals. Sepia is the best prescription in case of irritation and stitches-like sensations in the vagina. There is pain in the vagina during coition due to vaginal candidiasis.
Calcarea carbonica ostrearum (Calc.)
Common name: Carbonate of lime
Calcarea carb. is one of the best homeopathic remedies for vaginal candidiasis with milky white vaginal discharge. One key note symptom for prescribing Calcarea carb. is worsening of the vaginal discharge while passing urine. The vaginal discharge, accompanied by burning and intense itching in the genitals, calls for this remedy. This burning and itching gets worse before and after periods. Calcarea carb. is effective for redness in the vagina and vulva due to swelling in vaginal candidiasis.
Pulsatilla nigricans (Puls.)
Common name: Windflower
Pulsatilla is an effective remedy for vaginal candidiasis with a peculiar thick, creamy, and acrid vaginal discharge. There is intense burning and corrosive itching in the genitals with discharge.
Women who need Pulsatilla have vaginal discharge before, during, and after their periods. Backache with white discharge is a characteristic symptom of this remedy.
Helonias dioica chamaelirium (Helon.)
Common name: Unicorn root
Helonias is a homeopathic remedy for vaginal candidiasis with curdy deposits in the vulva. Other characteristic symptoms of Helonias include inflammation of private parts with swelling, burning, and redness. Intense heat and itching in the genitals due to vaginal candidiasis calls for this remedy.
These women complain of excessive weakness, tiredness, and prostration with white discharge. A highly marked characteristic of using Helonias is backache with vaginal infection.
Monilia albicans (Moni.)
Common name: Candida albicans
Monilia albicans gives efficient results in vaginal candidiasis with cracks or fissures in the vulva and vagina.
Constant itching with marked inflammation and swelling indicates Monilia albicans. In women with vesicular eruptions in the vulva or vagina, Monilia albicans is the best-suited remedy.
Causes of vaginal candidiasis
Candida fungus
Candida albicans is a normal yeast that resides in the vagina. The overgrowth can happen due to disruption of the balance of microorganisms in the vagina.
Antibiotics
Using antibiotics can disrupt the balance of microbes in your body. It includes those in the vagina, allowing Candida fungi to proliferate.
Hormonal changes
Hormonal fluctuations during pregnancy, menstruation, or menopause can make women more prone to vaginal candidiasis.
Weak immune system
Conditions or medications that weaken the immune system increase the risk of vaginal candidiasis.
Diabetes
Uncontrolled diabetes can lead to high blood sugar levels. This, in turn, can encourage vaginal candidiasis.
Diet
A diet stuffed with high sugar and refined carbohydrates can promote vaginal candidiasis.
Tight clothing
Wearing tight, non-breathable underwear can create a warm, moist environment around the genitals. This can favor yeast growth leading to vaginal candidiasis.
Douching
Douching is a process of washing out the inside of the vagina. This can disrupt the natural balance of microbes in your vagina. Ultimately increasing the risk of vaginal candidiasis.
Sexual activity
Sexual activity can transmit fungi from one partner to another.
Symptoms of vaginal candidiasis
Itching
The most common symptom of vaginal candidiasis is vaginal itching. Often, the itching is persistent and intense.
Burning
Women with vaginal candidiasis often feel a burning or stinging sensation. The pain gets intense during urination or sexual intercourse.
Abnormal vaginal discharge
A thick, white, and watery discharge is a characteristic symptom of vaginal candidiasis. It often resembles cottage cheese and is odorless.
Redness and swelling
The vulva and vaginal tissues may become red, swollen, and irritated due to fungal infection.
Pain
A general discomfort and pain in the vaginal area is common in vaginal candidiasis.
Soreness
There can be soreness and sensitivity in the vaginal region in vaginal candidiasis.
Treatment for vaginal candidiasis
Vaginal candidiasis is commonly treated with antifungal medications. There are various over-the-counter and prescription medications available for treatment. Here are some standard treatment options:
Over-the-counter (OTC) antifungal medications
Mild vaginal candidiasis is treated with OTC antifungal creams, ointments, or suppositories.
Prescription medication
In severe or recurrent yeast infections, a healthcare provider may prescribe stronger antifungal medications like creams, suppositories, or oral tablets.
Oral antifungal medications
In cases of complicated or recurrent vaginal candidiasis, an oral antifungal medication is prescribed.
Topical steroids
In cases of vaginal candidiasis with severe inflammation and discomfort, a topical steroid cream is used. It is often used in conjunction with antifungal medications to relieve symptoms.
It’s essential to complete the entire course of treatment, even if symptoms improve. Also, before you stop medications, ensure the infection is completely cleared.
Dietary changes for vaginal candidiasis
Avoid sugary foods
Yeast feeds on sugar. Thus, reducing your sugar intake in the form of refined sugars and sugary beverages can help. Follow a balanced, low-sugar diet.
Probiotics
Probiotics help maintain a healthy balance of microbes in your body. Consuming probiotic-rich foods like yogurt with live cultures can prevent vaginal candidiasis.
Hydration
Hydration is the key to flush out toxins and maintain overall health.
Limit antibiotic use
Avoid using antibiotics unnecessarily. Excess use of antibiotics can disrupt the balance of microorganisms in your body.
Avoid tight clothing
Wearing loose, breathable clothing can help prevent excess moisture and heat in the vaginal area.
Cotton innerwear
Choose cotton underwear. It allows for better air circulation in private parts. This helps keep the vaginal area dry.
Stress management
High-stress levels can weaken the immune system causing recurrent vaginal candidiasis. It makes you more susceptible to infections. Practicing stress-reduction techniques like deep breathing, meditation or yoga can be of help.
Good hygiene practices
Practicing good hygiene is the first step towards preventing vaginal candidiasis. Avoid using harsh soaps or scented products for vaginal wash. Gently clean using mild, unscented products.
Conclusion
Vaginal candidiasis is a fairly common condition in women. Overgrowth of the fungus results in candidiasis. Homeopathic remedies are effective and safe for treating vaginal candidiasis. These medicines inhibit the growth of yeast and improve your body’s immune system. Thus keep vaginal candidiasis at bay.
References
- Bitew A, Abebaw Y. Vulvovaginal candidiasis: species distribution of Candida and their antifungal susceptibility pattern. BMC Womens Health [Internet]. 2018 [cited 2023 Nov 5];18(1). Available from: http://dx.doi.org/10.1186/s12905-018-0607-z
- Jeanmonod R, Jeanmonod D. Vaginal Candidiasis. StatPearls Publishing; 2023.https://www.ncbi.nlm.nih.gov/books/NBK459317/
- Xu J, Schwartz K, Bartoces M, Monsur J, Severson RK, Sobel JD. Effect of antibiotics on vulvovaginal candidiasis: A MetroNet study. J Am Board Fam Med [Internet]. 2008 [cited 2023 Nov 5];21(4):261–8. Available from: https://pubmed.ncbi.nlm.nih.gov/18612052/
- Fidel PL Jr, Cutright J, Steele C. Effects of reproductive hormones on experimental vaginal candidiasis. Infect Immun [Internet]. 2000 [cited 2023 Nov 5];68(2):651–7. Available from: http://dx.doi.org/10.1128/iai.68.2.651-657.2000
- Talaei Z, Sheikhbahaei S, Ostadi V, Hakemi MG, Meidani M, Naghshineh E, et al. Recurrent vulvovaginal candidiasis: Could it be related to cell-mediated immunity defect in response to candida antigen? International Journal of Fertility & Sterility [Internet]. 2017 [cited 2023 Nov 5];11(3):134. Available from: http://dx.doi.org/10.22074/ijfs.2017.4883
- Mohammed L, Jha G, Malasevskaia I, Goud HK, Hassan A. The interplay between sugar and yeast infections: Do diabetics have a greater predisposition to develop oral and vulvovaginal candidiasis? Cureus [Internet]. 2021 [cited 2023 Nov 5];13(2). Available from: http://dx.doi.org/10.7759/cureus.13407
- Santana IL, Gonçalves LM, Vasconcellos AA de, da Silva WJ, Cury JA, Cury AADB. Dietary carbohydrates modulate candida albicans biofilm development on the denture surface. PLoS One [Internet]. 2013 [cited 2023 Nov 5];8(5):e64645. Available from: http://dx.doi.org/10.1371/journal.pone.0064645
- Elegbe IA, Botu M. A preliminary study on dressing patterns and incidence of candidiasis. Am J Public Health [Internet]. 1982 [cited 2023 Nov 5];72(2):176–7. Available from: http://dx.doi.org/10.2105/ajph.72.2.176
- Shaaban OM, Abbas AM, Moharram AM, Farhan MM, Hassanen IH. Does vaginal douching affect the type of candidal vulvovaginal infection? Med Mycol [Internet]. 2015 [cited 2023 Nov 5];53(8):817–27. Available from: https://pubmed.ncbi.nlm.nih.gov/26129887/
- Abhishek K, Kombade S, Mittal P, Sharma C, Singh P, Nag V. Antifungal profile of vulvovaginal candidiasis in sexually active females from a tertiary care hospital of Western Rajasthan. J Family Med Prim Care [Internet]. 2021 [cited 2023 Nov 5];10(1):398. Available from: http://dx.doi.org/10.4103/jfmpc.jfmpc_1124_20
- Cohen MS. Approach to the patient with a sexually transmitted disease. In: Goldman’s Cecil Medicine. Elsevier; 2012. p. 1796–800. https://linkinghub.elsevier.com/retrieve/pii/B9781437716047002931
- Multicentre Study Group. Treatment of vaginal candidiasis with a single oral dose of fluconazole. Eur J Clin Microbiol Infect Dis [Internet]. 1988 [cited 2023 Nov 5];7(3):364–7. Available from: https://pubmed.ncbi.nlm.nih.gov/2842157/
- Phillips NA, Bachmann G, Haefner H, Martens M, Stockdale C. Topical treatment of recurrent vulvovaginal candidiasis: An expert consensus. Womens Health Rep (New Rochelle) [Internet]. 2022 [cited 2023 Nov 5];3(1):38–42. Available from: http://dx.doi.org/10.1089/whr.2021.0065
- Xie HY, Feng D, Wei DM, Mei L, Chen H, Wang X, et al. Probiotics for vulvovaginal candidiasis in non-pregnant women. Cochrane Libr [Internet]. 2017 [cited 2023 Nov 5];2017(11). Available from: http://dx.doi.org/10.1002/14651858.cd010496.pub2
- Chen Y, Bruning E, Rubino J, Eder SE. Role of female intimate hygiene in vulvovaginal health: Global hygiene practices and product usage. Womens Health (Lond Engl) [Internet]. 2017 [cited 2023 Nov 5];13(3):58–67. Available from: http://dx.doi.org/10.1177/1745505717731011
- Meyer H, Goettlicher S, Mendling W. Stress as a cause of chronic recurrent vulvovaginal candidosis and the effectiveness of the conventional antimycotic therapy. Mycoses [Internet]. 2006 [cited 2023 Nov 5];49(3):202–9. Available from: https://pubmed.ncbi.nlm.nih.gov/16681811/