Approximately 1.4 million Indians struggle with inflammatory bowel disease (IBD), which includes ulcerative colitis. People between 15-30 years are more prone to develop ulcerative colitis.
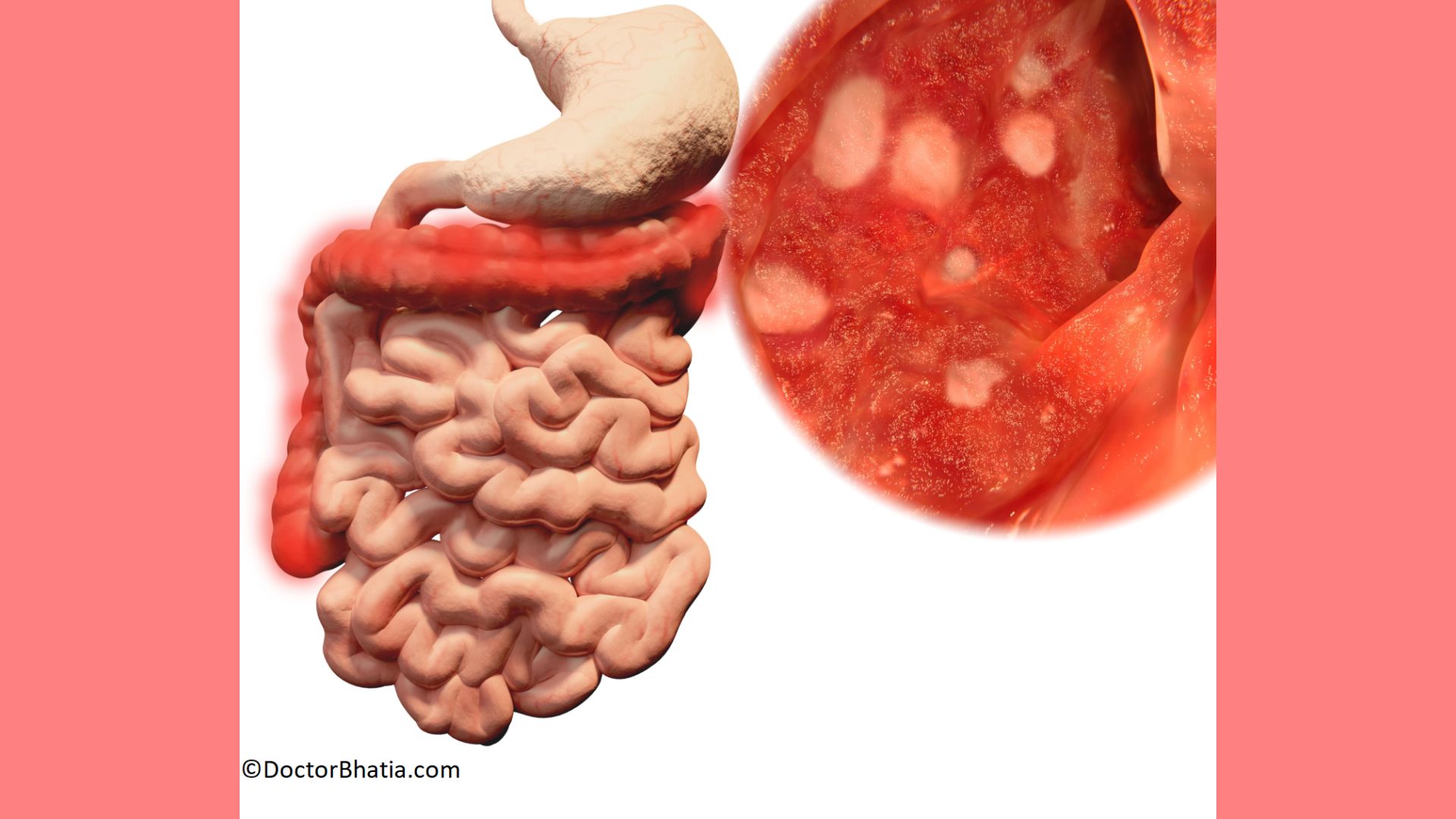
Your colon lining develops tiny microscopic wounds due to inflammation in ulcerative colitis. These wounds are known as ulcers. Ulcers in ulcerative colitis start in the rectum and spread upward. Gradually, these ulcers affect the entire colon. These ulcers could bleed and discharge pus and mucous.
Homeopathic medicines treat ulcerative colitis by correcting overactive immune mechanisms. However, the extent of improvement will vary depending on several factors. These factors include duration, intensity, and stage at which homeopathy treatment is started.
Role of homeopathy in ulcerative colitis
Homeopathy is highly effective in the case of ulcerative colitis. In ulcerative colitis, the autoimmune response damages the gut lining, causing ulcers. Homeopathy acts by correcting the hyper-responsive immune system. This corrects the root cause of ulcerative colitis.
Also, homeopathic medicines reduce the severity, frequency, and relapses of ulcerative colitis. Thus, it safely and gently gives you long-term relief from ulcerative colitis. The best part is with homeopathy, you can avoid ulcerative colitis surgery.
Top five homeopathic remedies for ulcerative colitis
Mercurius solubilis (Merc.)
Common name: Quicksilver
Merc. sol. is one of the top-grade medicines for ulcerative colitis with blood in stools. This remedy is indicated for frequent loose stools.
Merc. sol. offers great help in cases of ulcerative colitis with excessive burning and intense pain in the rectum. These people have a constant urge to evacuate the bowels. However, even after passing stool several times, there is no relief.
Nux vomica (Nux-v.)
Common name: Poison nut
Nux vomica is beneficial in ulcerative colitis due to irregular eating habits. In ulcerative colitis, due to excessive work stress this remedy suits well.
This remedy is indicated in those with an ineffective urge to pass stool. These people have to strain during bowel movements. It is also the best choice of homeopathic remedy in ulcerative colitis, where stool is passed bit by bit throughout the day, but still, the urge to defecate continues.
Nitricum acidum (Nit-ac.)
Common name: Nitric acid
Nitric. acid. treats ulcerative colitis with intense pain in the rectum while passing stool. It is indicated for tearing or cutting pain in the abdomen. These people have to strain to the extent that their rectum feels like it is torn and yet passes very little stool.
Nitric. acid. relieves abdominal pains that are violent, tearing, and cutting in nature. This abdominal pain continues for hours after stool. This remedy works best in case of profuse, bright red bleeding along with stool.
Aloe socotrina (Aloe.)
Common name: Socotrine aloes
Aloe socotrina is an excellent homeopathic remedy for ulcerative colitis with an urgency to pass stool. The patient feels an urgency to pass stool more in the morning, after eating or drinking.
This remedy works well for those with a constant bearing down sensation in the rectum. It helps in cases of ulcerative colitis with intense burning in the anus and rectum. Another characteristic feature of using Aloe soc. is a sense of uncertainty in the rectum while passing flatus; not sure if gas or stool will come. Stool passes without any effort with jelly-like mucus in the stool. This remedy works wonders in people with lumpy, watery, and jelly-like stools.
Phosphorus (Phos.)
Common name: Phosphorus
Phosphorus is prescribed for ulcerative colitis with bloody diarrhea and weakness. There is often extreme exhaustion after passing stool. Stools are often copious, gushing, and watery. This is a significant medicine for frequent stools with painless and rectal bleeding. The bleeding is copious and bright red.
These people complain of watery, yellowish stools that have an offensive odor. There can be cramping pain in the rectum on passing stool.
Causes for ulcerative colitis
Although the exact cause is unknown, ulcerative colitis can be due to genetic, environmental, and immunological factors.
Genetics
Family history increases the risk of developing ulcerative colitis. This suggests the significant role of genetic components.
Immune system
Ulcerative colitis is believed to be an autoimmune disease. Here, the immune system targets the lining of your colon. This leads to inflammation, causing ulcerative colitis.
Environmental triggers
Environmental factors can trigger or exacerbate ulcerative colitis. These factors include infections or exposure to environmental substances.
Gut microbes
The altered composition of the gut microbiota (microorganisms in the intestines) plays a role in developing ulcerative colitis.
Smoking
Smoking is known to be a high-risk factor for ulcerative colitis. Studies have shown that smoking can cause inflammation in the gut lining.
Symptoms of ulcerative colitis
Symptoms of ulcerative colitis can vary from mild to severe. Ulcerative colitis is a condition with frequent flare-ups and remission. Also, the intensity and combination of symptoms can vary from person to person. Common symptoms of ulcerative colitis include:
Diarrhea
The hallmark symptom of ulcerative colitis is diarrhea. Often, people complain of frequent, urgent bowel movements with loose or bloody stools.
Abdominal pain
Crampy abdominal pain is often experienced by those who have ulcerative colitis. Abdominal cramps are often felt during bowel movements.
Rectal bleeding
Another characteristic symptom of ulcerative colitis is rectal bleeding. Blood is either seen in the stool or pot or visible on wiping.
Urgency to defecate
A sudden and strong urge to pass bowels is seen in most cases of ulcerative colitis.
Tenesmus
In ulcerative colitis, there is a feeling of incomplete bowel emptying. Tenesmus is often accompanied by the need to pass stool frequently.
Fatigue
As a response to chronic inflammation, you might feel fatigue in ulcerative colitis.
Loss of appetite
Inflammation in ulcerative colitis leads to reduced appetite and nutrient malabsorption.
Weight loss
Decreased appetite can result in weight loss.
Joint pain
Ulcerative colitis is often accompanied by joint pain or arthritis-like symptoms.
Skin and eye problems
Some people may experience skin rashes, eye inflammation, or other extraintestinal symptoms.
Anemia
Chronic bleeding in the colon can lead to iron deficiency anemia in several cases of ulcerative colitis.
Treatment for ulcerative colitis
Ulcerative colitis is treated with a combination of medical therapies and lifestyle modifications. The treatment aims to reduce inflammation, control symptoms, and prevent flare-ups. Here are some common treatment options to manage ulcerative colitis:
Medications
- Anti-inflammatory drugs
Medications like aminosalicylates are used to reduce inflammation in the colon. These medications are often prescribed for mild to moderate cases of ulcerative colitis.
- Corticosteroids
Corticosteroids are prescribed to control severe inflammation during flare-ups. However, these are not suitable for long-term use due to side effects.
- Immunomodulatory medicines
Medications like azathioprine and 6-mercaptopurine are used to suppress the abnormal immune response.
Supplements
Nutrient absorption is compromised in the case of ulcerative colitis. Talk to your doctor about whether you need any vitamin or mineral supplements.
Biologics
Biologics like anti-TNF agents, target specific proteins in the immune system. These are used in moderate to severe cases of ulcerative colitis that don’t respond to other treatments.
Surgery
In severe cases of ulcerative colitis or when medical treatments are ineffective, surgery is advised. Surgical options include
- Total colectomy that involves removing the colon
- Ileal pouch-anal anastomosis (IPAA) involves the removal of the large intestine and rectum
- Ileostomy
Dietary management for ulcerative colitis
- Avoid trigger foods
Identify and avoid foods that worsen ulcerative colitis symptoms. Common foods triggering flare-ups include caffeine, alcohol, high-fiber foods, spicy foods, dairy products, and fried foods.
- Low-FODMAP diet
A low-FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet is effective in people with ulcerative colitis. This diet restricts certain types of carbohydrates that can cause digestive distress.
- Small, frequent meals
Eating smaller meals more frequently can decrease the strain on your digestive system. This helps minimize symptoms of ulcerative colitis.
- Hydration
Diarrhea in ulcerative colitis can lead to fluid loss. Staying well-hydrated helps, especially during flare-ups.
Lifestyle management for ulcerative colitis
- Stress reduction
High stress levels can worsen symptoms. Practice stress-reduction techniques like meditation, yoga, deep breathing exercises, or hobbies that relax you.
- Regular exercise
Regular physical activity helps maintain overall health and improve your gut health.
- Smoking cessation
If you have IBD, quitting smoking is essential. Smoking can worsen ulcerative colitis symptoms.
Conclusion
Ulcerative colitis can disrupt your routine activities. Its treatment involves a multifaceted approach combining medical treatment, dietary and lifestyle modifications.
Homeopathy is the recommended mode of treatment for ulcerative colitis. Constitutional homeopathic medicines for ulcerative colitis can provide symptomatic relief and prevent the recurrence of the disease. This holistic approach can manage this condition and help you live a life free from ulcerative colitis.
References
- Kedia S, Ahuja V. Epidemiology of inflammatory bowel disease in India: The great shift east. Inflamm Intest Dis [Internet]. 2017 [cited 2023 Nov 2];2(2):102–15. Available from: http://dx.doi.org/10.1159/0004655
- Lynch WD, Hsu R. Ulcerative Colitis. StatPearls Publishing; 2023.https://www.ncbi.nlm.nih.gov/books/NBK459282/
- Researchgate.net. [cited 2023 Nov 2]. Available from: https://www.researchgate.net/publication/314010486_Homoeopathic_treatment_of_ulcerative_Colitis_A_case_report
- Researchgate.net. [cited 2023 Nov 2]. Available from: https://www.researchgate.net/publication/360881584_A_Case_of_Irritable_Bowel_Syndrome_Treated_by_Nux_Vomica_A_Case_Report
- No title [Internet]. Google.com. [cited 2023 Nov 2]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6487890/#:~:text=8%E2%80%9314%25%20of%20patients%20with,risk%20of%20developing%20the%20disease.
- Wen Z, Fiocchi C. Inflammatory bowel disease: Autoimmune or immune-mediated pathogenesis? Clin Dev Immunol [Internet]. 2004 [cited 2023 Nov 2];11(3–4):195–204. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2486322/
- Abegunde AT, Muhammad BH, Bhatti O, Ali T. Environmental risk factors for inflammatory bowel diseases: Evidence based literature review. World J Gastroenterol [Internet]. 2016 [cited 2023 Nov 2];22(27):6296. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4945988/
- Shen Z-H, Zhu C-X, Quan Y-S, Yang Z-Y, Wu S, Luo W-W, et al. Relationship between intestinal microbiota and ulcerative colitis: Mechanisms and clinical application of probiotics and fecal microbiota transplantation. World J Gastroenterol [Internet]. 2018 [cited 2023 Nov 2];24(1):5–14. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5757125/
- Verschuere S, De Smet R, Allais L, Cuvelier CA. The effect of smoking on intestinal inflammation: What can be learned from animal models? J Crohns Colitis [Internet]. 2012;6(1):1–12. Available from:https://www.sciencedirect.com/science/article/pii/S187399461100256X
- Nakashima J, Preuss CV. Mesalamine (USAN). StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK551714/#:~:text=Mesalamine%2C%20also%20known%20as%205,resection%20of%20the%20affected%20bowel.
- Mahadevan U. Medical treatment of ulcerative colitis. Clin Colon Rectal Surg [Internet]. 2004 [cited 2023 Nov 2];17(01):7–19. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2780076/
- Timmer A, Patton PH, Chande N, McDonald JWD, MacDonald JK. Azathioprine and 6-mercaptopurine for maintenance of remission in ulcerative colitis. Cochrane Libr [Internet]. 2016 [cited 2023 Nov 2];2016(5). Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7034525/
- Park SC, Jeen YT. Current and emerging biologics for ulcerative colitis. Gut Liver [Internet]. 2015 [cited 2023 Nov 2];9(1):18–27. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4282853/
- Campmans-Kuijpers MJE, Dijkstra G. Food and food groups in inflammatory bowel disease (IBD): The design of the Groningen anti-inflammatory diet (GrAID). Nutrients [Internet]. 2021 [cited 2023 Nov 2];13(4):1067. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8064481/
- Grammatikopoulou MG, Goulis DG, Gkiouras K, Nigdelis MP, Papageorgiou ST, Papamitsou T, et al. Low FODMAP diet for functional gastrointestinal symptoms in quiescent inflammatory bowel disease: A systematic review of randomized controlled trials. Nutrients [Internet]. 2020 [cited 2023 Nov 2];12(12):3648 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7760970/
- Sun Y, Li L, Xie R, Wang B, Jiang K, Cao H. Stress triggers flare of inflammatory bowel disease in children and adults. Front Pediatr [Internet]. 2019 [cited 2023 Nov 2];7. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6821654/#:~:text=Chronic%20stress%20can%20cause%20excessive,production%20of%20poisons%20(87).
- Bilski J, Brzozowski B, Mazur-Bialy A, Sliwowski Z, Brzozowski T. The role of physical exercise in inflammatory bowel disease. Biomed Res Int [Internet]. 2014 [cited 2023 Nov 2];2014:1–14. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4022156/
- Bastida G. Ulcerative colitis in smokers, non-smokers and ex-smokers. World J Gastroenterol [Internet]. 2011 [cited 2023 Nov 2];17(22):2740. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3122262/